our health programs
Data to June 2021
Following on from 2020, the first six months of 2021 saw Opportunity International Australia’s health program extend into new areas, form new partnerships and provide new services in response to the COVID-19 crisis.
With the support of the Opportunity community, we were able to make a significant difference in the lives of those affected by illness, loss, lockdowns, and threatened livelihoods.
We supported access to vaccinations, safe isolation, mental health care, primary health care, remote care delivered by local partners, and education delivered by community Health Leaders.
Opportunity’s health program is supported by the Australian Government through the Australian NGO Cooperation Program (ANCP).
Responding to COVID-19’s second wave in India
In May 2021, at the peak of the second wave of COVID-19, India became the epicentre of the global pandemic with more than 400,000 new cases reported in a single day. Second in total case numbers only to the USA and recording 27 million cases by late May, the healthcare system was overwhelmed, with reduced supplies of essential treatments.
Opportunity began working with new and existing partners in India to respond to the crisis. We’re incredibly grateful to our supporters to have raised over AU$2 million in this work.
A snapshot of the impact of Opportunity’s five-point COVID-19 rapid-response strategy across 1,200 rural and remote villages:
1. To prevent infection in vulnerable populations at risk, we tackled rampant misinformation through SMS, WhatsApp, comics, posters, voice messages and in-person meetings where possible.
Impact: 140,000 people reached every day by Health Leaders delivering critical COVID-19 education, with some fluctuation given the state of local lockdowns. Posters were put up and audio messages played in shops across 500 rural villages. SMS messages and two-minute videos were circulated widely via WhatsApp.
2. For those with mild symptoms or exposure to COVID-19, our partners distributed food ration kits, sanitary kits and medicine so they could isolate safely.
Impact: More than 700 people who had COVID-19 symptoms isolated in 75 village-level quarantine centres. These centres were located in unused school buildings, churches or government offices to help adults with mild COVID-19 symptoms isolate safely, since many live in single-room homes and/or use a shared toilet. At these centres, they received sanitary kits, medicine (such as paracetamol) and nutritional supplements (such as eggs, milk, vegetables and dahl). In addition, 1,000 ration kits were distributed to families in urban slums and rural communities. Medicine kits and ration kits were distributed in 748 villages.
3. To manage COVID-19 cases and mental health at home, our partners provided remote care through telemedicine (via helpline and mobile app).
Impact: Our partners provided free telemedicine through 336 telemedicine clinics co-located with branch offices or directly through a mobile app available to 1 million households. In addition, they provided a 24/7 multilingual public toll-free helpline with three components;
- Helpline: this new service grew to cover 60,000 calls/month.
- Dial-in information hotline with call-back option (50-100 calls/day): this service was used by Opportunity’s partner in the first wave as well.
- Telecounselling service: 60 Health Leaders were trained as telecounsellors to provide mental health support and grief counselling.
4. For people with worsening COVID-19 symptoms, our partners provided emergency transport and basic primary health services in underserved areas while supporting the public health system.
Impact: We worked to ensure that over 1 million rural households had access to emergency transport if they experienced critical COVID-19 symptoms, and provided 100 oxygen concentrators to community health centres. In addition, we set up mobile medical vans to serve over 4,800 patients per month in containment zones in the urban slums of Pune, in the hardest-hit state of Maharashtra.
5. To expedite mass vaccinations to improve immunity, Opportunity’s partners collaborated with local governments to organise and facilitate vaccination camps given their trusted presence in local communities where they provide microfinance services.
Impact: Our partners facilitated over 1,900 vaccination camps (administering 200,000 doses of vaccines) with a focus on health equity and serving high-need communities and populations, including tribal communities, other remote rural communities as well as seniors, disabled and transgender groups.
While vaccinations are provided by the government free of charge, it costs approximately AU$2 (INR 110) on direct transport and indirect lost wages for a person to get vaccinated. The vaccination camps are set up in local villages, eliminating the need for travel. Given a vaccination camp reaches 125 people, the camp creates an economic benefit of AU$250 (INR 13,800), while only costing Opportunity’s microfinance partners AU$15-20 to run each camp.
Voice of the program
Health Leader education helped me protect my son from illness’

Rani lives in Tangail district, Bangladesh, with her husband and young son, Yasin. Rani’s husband makes garments, earning a meagre income, while Rani looks after their son. Yasin was often ill and Rani could not work out why he was so prone to frequent bouts of vomiting and diarrhea. It got so bad that Yasin’s life was in danger, and he was admitted to hospital for treatment, which posed a significant financial burden for this family living in poverty.
With funding through the 2020-2021 Australian NGO Cooperation Program, Opportunity’s implementing partner in Bangladesh trained 200 women to provide basic health education to over 40,000 households in 617 remote rural communities.
Kulsum was one of the Health Leaders trained. She completed a course covering 25 basic health education modules, including hand washing, environmental health and hygiene, and how stool- and water-borne disease is spread.
Kulsum was paid a stipend to visit households in her community and teach families how to improve their health.
Rani was eager and quick to learn, soon understanding the health benefits of a birth plan, neonatal care, early and regular prenatal care, adolescent healthcare – and especially keeping her house and surroundings clean. She bought a play mat so that Yasin wouldn’t play on the dirt in the courtyard where chickens and ducks roamed free.
She practiced other healthy habits in her home each day, including proper waste disposal and hand washing. Rani is thankful for the improved health knowledge she has gained.
She is now able to make the changes necessary to see a significant improvement in her family’s health, prevent illness and to avoid unnecessary health expenses in the future.
Strategic direction
Contributing to sustainable development

India
Opportunity supported the establishment of 18 e-clinics in India. Women previously trained as Health Leaders were provided with further training to equip them to run the e-clinics. The women were provided with equipment to assess patients’ health indicators, such as blood oxygen saturation and blood pressure.
If required, the Health Leaders at the clinics facilitated consultations with qualified health professionals remotely using a digital platform. Between April and June 2021, 14,597 patients in remote rural locations were able to speak with a doctor through the e-clinics. In the same period, an additional 30,081 people were helped to reach a doctor over the phone.
Every digital consultation represents a cost saving to the patient. There is a transport cost saving as the patients don’t need to travel long distances to access a doctor. There is an opportunity cost saving, as patients don’t need to leave their businesses unattended, and there is a cost saving in accessing healthcare in a timely manner, rather than waiting until the patient deteriorates to the point where significant and costly medical intervention is needed.

Indonesia
In Indonesia, 34# women completed their internship as Health Leaders and delivered six modules of basic health education over six months to their communities. The module covered topics on nutrition, disease control (including COVID-19 and TB), women’s health, maternal and child health, and adolescent health. The curriculum aligned with the Indonesian Government’s Program on Health Promotion, incorporating some of their posters to reinforce the health education covered in each module.
The growth of the health education program in Indonesia was significantly hampered due to COVID-19-related restrictions and illness, with new daily case numbers exceeding 20,000 by the end of June. Despite these setbacks, the Health Program team at Opportunity’s implementing partner recruited and trained nine new staff members in preparation to grow the program by training another 240* Health Leaders in eight branch locations across East, West and Central Java, as well as Petir in Lebak Regency, Banten. Lebak Regency in Banten has been prioritised for the health program due to the high number of maternal health problems prevalent there, including high maternal and infant mortality rates.
Bangladesh
Community Health Education curriculum content was adapted to include information on COVID-19 and contextualised to local conditions. Training modules and related materials (including booklets and flashcards) were amended to include COVID-19 awareness and prevention information. Health Leaders cascaded the health education to community members on COVID-19 disease awareness, prevention, identification, testing and available treatment options.
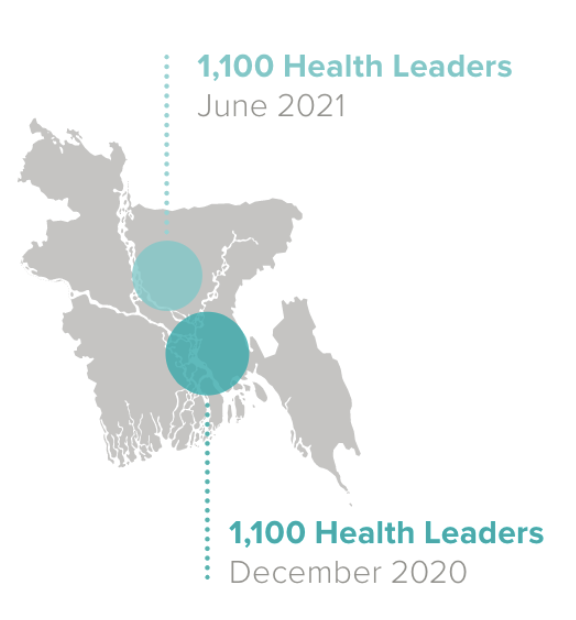
In Bangladesh, from 10 November 2020 to 3 June 2021, Health Leaders reached 40,209 women at their homes in 617 local villages in Tangaildistrict, with 25 modules of basic health education.
COVID-19 interrupted the training of Health Leaders in 2021. From 2022, measurement and impact reporting will change to reflect our expanding health program.
Case study
Addressing COVID-19 misinformation through education
Opportunity worked collaboratively with external health and development consultants to develop culturally appropriate COVID-19 second wave education materials.
The materials focused on mental health and vaccinations and were designed to fight myths and misinformation. Four new 30-minute modules of participatory education were developed for our Health Leaders, and online Train the Trainer sessions provided to our partners in India.
Each module includes three to five pictures plus a facilitator guide, to be used where microfinance clients gather to make repayments on their loans.
Materials were adapted to be locally relevant for communities in Indonesia, Bangladesh and Nepal, as well as India.
This project is supported by the Australian Government through the Australian NGO Cooperation Program (ANCP).
# These women completed their training and were counted in a previous reporting period.
*These women will complete their training and be counted in the next reporting period.
Impact Stories
Your support is empowering these women—and millions more like them—to build a healthier future their families.

"Prevention is better than cure."
– Jessica Carter, Asia Health Program Director
How important is health? We asked Jessica a few questions about how healthcare is helping families leave poverty behind.

How our partners have responded to the COVID-19 pandemic
Opportunity’s microfinance partners have introduced new initiatives in response to coronavirus and to support families living in poverty during this time.

"...as we started meeting regularly, it became like a family."
– Usha Devi, Uttar Pradesh
Usha is a BCP—a Basic Care Provider—not quite a paramedic or nurse, but more than a first aid responder. BCPs provide an essential health service to people living in rural India.

The COVID-19 lockdown for 1.3 billion people in India posed a very different situation than lockdown in Australia. Jessica Carter, our Asia Health Program Director—based in Hyderabad, India—explains.